for Health Care Providers
Diagnosis - Non-Alcoholic Fatty Liver
The most common chronic liver disease in U.S. affecting 2.7 million Veterans, NAFLD is a leading cause of cirrhosis and hepatocellular carcinoma and a leading indication for liver transplantation.[1,2,3] In addition, having NAFLD increases the risk of developing diabetes, cardiovascular disease, and kidney disease (Figure 1). [4,5,6]
Early identification by primary care providers and implementation of lifestyle modifications in patients with evidence of fibrosis progression is critical.
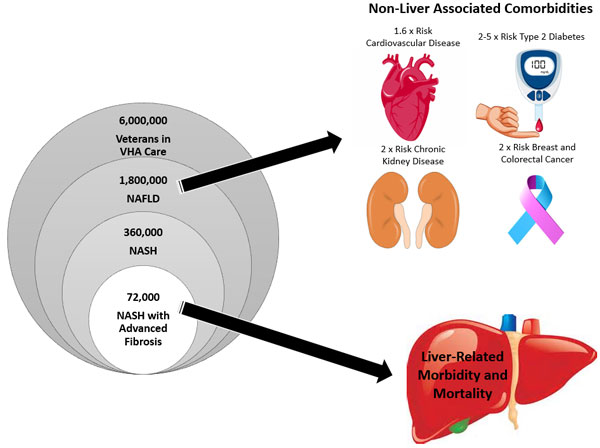
Figure 1: Estimated prevalence of NAFLD in VA, and increased risk of comorbidities among patients with NAFLD. (Veterans in care is estimated from VA data). Figure source: VA NAFLD Considerations
Patients who are overweight or obese and have persistently elevated ALT or fatty liver on imaging should be evaluated for NAFLD.
Diabetic patients should have a liver panel every 1-2 years. Patients with an elevated ALT (for >6 months) with no other etiology for liver injury (e.g., medications, viral hepatitis B or C, hemochromatosis, etc.) should be assessed for fibrosis risk using an online Fibrosis-4 score (FIB-4) calculator (example: https://www.mdcalc.com/fibrosis-4-fib-4-index-liver-fibrosis![]() ).
).
A healthy ALT is defined as:
- Men= ≤30 IU/L
- Women= ≤20 IU/L
- These are general guidelines. ALT can vary according to the autoanalyzer used.
What is FIB-4?
Non-invasive liver fibrosis score which is calculated using patient age, ALT, AST, and platelet count (example: https://www.mdcalc.com/fibrosis-4-fib-4-index-liver-fibrosis![]() ).
).
FIB-4 Score >2.67 in patients with NAFLD has 80% positive predictive value for detecting advanced fibrosis.[7] These patients should be further assessed for a diagnosis and referred to GI if indicated.
FIB-4 should not be used in patients <35 years old. Age >65 may elevate FIB-4.
Patients with suspected liver fibrosis (≥F2 fibrosis) based on FIB-4 merit a hepatology/GI referral for further assessment.
Figure 2: FIB-4 Risk Stratification and Referral to GI
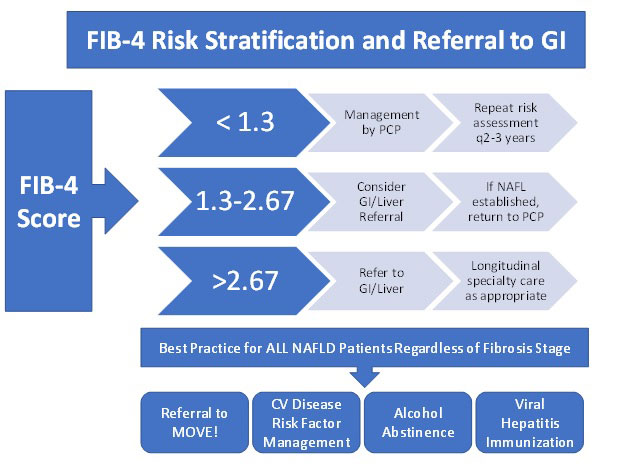
Patients should be assessed for severity of liver fibrosis using the FIB-4 score or other algorithm that uses clinical information and/or routine blood tests. FIB-4 score can be calculated from patient's age, AST, ALT, and platelet count. Among patients >65 years old, age may elevate FIB-4 score in the absence of significant fibrosis; for these patients, a FIB-4 <2.0 excludes advanced fibrosis. FIB-4 should not be used to estimate liver fibrosis among patients <35 years of age. FIB-4 is a predictive tool for staging liver fibrosis and should not be the only tool used to diagnose NAFLD. Figure source: VA NAFLD Considerations.[9]
Diagnosis
A diagnosis of NAFLD should be considered in patients with metabolic syndrome, obesity, and/or diabetes, who have:[8,9]
- Elevated liver transaminase (ALT or AST)
- No other identified cause of liver disease
- Viral hepatitis
- Alcohol use. Classically, the diagnosis of NAFLD required exclusion of significant alcohol use. Currently, it is accepted that patients who drink alcohol and have obesity, diabetes, or metabolic syndrome may have fat in the liver from NAFLD as well as from alcohol use.
- Parenteral nutrition
- Medications (e.g., corticosteroids, methotrexate, diltiazem, amiodarone, tamoxifen, highly active antiretroviral therapy)
- Fatty liver on imaging
References
- Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 2015; 148: 547- 555.
- Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease - Estes - 2018 - Hepatology - Wiley Online Library

- Projected increase in obesity and non-alcoholic-steatohepatitis-related liver transplantation waitlist additions in the United States - PubMed (nih.gov)

- Epidemiology and Natural History of Nonalcoholic Fatty Liver Disease - PubMed (nih.gov)
 (did not use ref 1 in the VA considerations - this is more recent).
(did not use ref 1 in the VA considerations - this is more recent). - Non-alcoholic fatty liver disease, the metabolic syndrome and the risk of cardiovascular disease: the plot thickens - PubMed (nih.gov)
 (same as 7 in VA considerations)
(same as 7 in VA considerations) - Cause, Pathogenesis, and Treatment of Nonalcoholic Steatohepatitis | NEJM
 (same as ref 9 in VA Considerations)
(same as ref 9 in VA Considerations) - Shah AG, Lydecker A, Murray K, Tetri BN, Contos MJ, Sanyal AJ. NASH Clinical Research Network. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7(10):1104-1112. [PMC free article
 ] [PubMed
] [PubMed ]
] - The Diagnosis and Management of Non-Alcoholic Fatty Liver Disease

- Practice Guidance from the American Association for the Study of Liver Diseases; Hepatology, 2018
- VA NAFLD Treatment Considerations. Internal document.




















