for Health Care Providers
How to Diagnose Cirrhosis - Cirrhosis
Identifying the presence of cirrhosis is essential in any patient with chronic liver disease. Making the diagnosis of cirrhosis will affect management and follow-up.
Key concepts
- Cirrhosis is the end stage of any chronic liver disease, such as hepatitis B, hepatitis C, alcohol-related liver disease, or metabolic dysfunction-associated steatotic liver disease
-
Clinical stages of cirrhosis: compensated and decompensated
- Patients with compensated cirrhosis may have gastroesophageal varices, but they never developed complications such as ascites, hepatic encephalopathy or variceal hemorrhage. The diagnosis of cirrhosis can usually be established without a liver biopsy, using clinical findings, imaging, lab tests and/or elastography
- Decompensated cirrhosis is characterized by the presence or development of ascites, variceal hemorrhage, or hepatic encephalopathy; a liver biopsy is rarely needed to confirm cirrhosis
Key recommendations
- Cirrhosis should be investigated in patients with chronic (>6 months in duration) abnormalities in liver enzymes and/or in patients in whom risk factors for cirrhosis are present: alcohol use disorder, hepatitis C, hepatitis B, obesity, and metabolic syndrome (even in the absence of liver enzyme abnormalities)
-
The following can help support the diagnosis of cirrhosis:
- Careful physical exam
- Appropriate laboratory tests
- Appropriate imaging tests
- Liver stiffness measurements
- However, physical exam, laboratory tests, and radiology tests (clinical findings) all may yield entirely normal results in a patient with compensated cirrhosis
- Liver biopsy (an invasive method) is required to establish (or exclude) the diagnosis of cirrhosis when there is high suspicion but absence of non-invasive findings
The diagnosis of decompensated cirrhosis is usually easy and straightforward. However, for compensated cirrhosis, a combination of clinical judgement, laboratory tests (e.g. FIB-4, imaging finding) should be used. Finally, elastography is the best non-invasive assessment of fibrosis.
Physical exam findings suggestive of decompensated cirrhosis (difficult to diagnose compensated cirrhosis with physical exam):
| Exam Finding | Example |
|---|---|
| Bitemporal muscle wasting | Loss of muscle mass in the temporal area 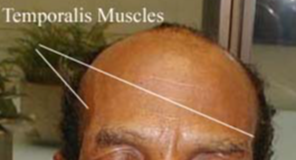 |
| Spider angioma | Blood vessel formation on the skin of the chest, back and face in the shape of a spider that fill from the center outward when blanched  |
| Palmar erythema | Redness on the palms of the hands  |
| Ascites | Fluid accumulation in the abdomen  |
| Abdominal collaterals (caput medusae) | Large venous collateral drainage on the surface of the abdomen 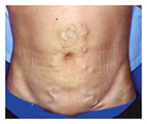 |
| Palpation/percussion |
|
Laboratory findings suggestive of cirrhosis:
- Platelet count < 150,000 (if no other explanation)
- Albumin < 3.5 mg/dL (if no albuminuria, malnutrition)
- AST > ALT
- INR > 1.2
- Bilirubin > 1.5 mg/dL (very non-specific, rule out Gilbert syndrome)
- FIB-4
 or
APRI
or
APRI scores calculated using age, AST, ALT, and/or platelet count (high negative predictive value)
scores calculated using age, AST, ALT, and/or platelet count (high negative predictive value)
- Specialized tests such as Enhanced Liver Fibrosis (not widely available)
Imaging findings (abdominal ultrasound, CT, or MRI) suggestive of cirrhosis:
- Nodular surface of the liver (subjective)
- Splenomegaly
- Collaterals or varices
- Enlarged caudate lobe/left lobe of the liver
- Shrunken right lobe of the liver
- Ascites
Elastographic findings suggestive of cirrhosis:
-
Transient elastography (Fibroscan®) is a point-of-care method to measure liver stiffness (LS)
- Most reliable non-invasive test for diagnosis of suspected cirrhosis
- Most useful for excluding cirrhosis
- LS can be falsely elevated e.g., non-fasting, aminotransferases >150 IU/mL, fluid accumulation from cardiac or renal dysfunction, and pulmonary hypertension.
- Other methods to measure liver stiffness include acoustic radiation force impulse (ARFI) and magnetic resonance elastography (MRE), but they are not point-of-care and have different cutoffs
- Combination of LS measurement and platelet count can have both diagnostic and prognostic values




















